Sub-par care and poor staffing are to blame, say health officials.
Skilled nursing homes and long-term care facilities are taking on a progressively larger role in the care of seriously ill patients who previously would have had prolonged hospital stays. According to a recent article in The New York Times, public health officials say these facilities are not succeeding in suppressing the spread of drug-resistant germs, including the fatal fungus Candida auris, that have affected hundreds of seriously ill nursing home patients.
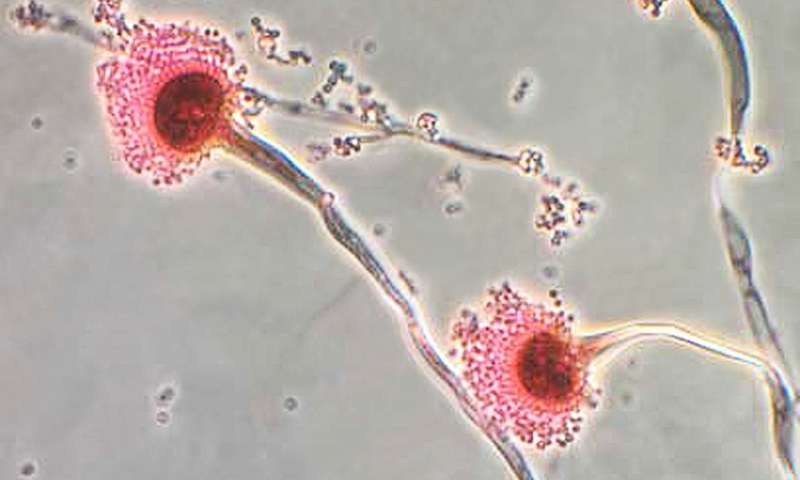
The overuse of antibiotics has been blamed for the drug-resistance of certain irrepressible infections contracted by nursing home patients. Among these infections is C. auris, a highly contagious fungus that is particularly difficult to contain. It has affected nearly 800 Americans since arriving in the country four years ago, and half of those infected died within 90 days. According to health officials, the germs of C. auris and other drug-resistant infections can reside without symptoms on the skin or within the bodies of nursing home patients, making them easily—and invisibly—spread. The protocol for preventing the spread of these germs to other patients or to visiting family members requires unvarying diligence, and it is here, says the Times, where long term care and nursing facilities go wrong.
Due to financial incentives set by Medicare, nursing homes and long term care facilities accept severely ill patients with increasing frequency—including especially vulnerable patients on ventilators—even if these facilities are poorly staffed or ill equipped to handle them. It is often instances of poor care and low staffing issues that interfere with a facility’s implementation of measures to mitigate the spread of infection:
- The invisible colonization of germs on or within patients’ bodies makes it easy for germs to spread to beds and rooms. The Times noted instances of failures to post warning signs outside of infected rooms to quarantine them.
- The containing of drug-resistant infections is often a matter of limiting the exposure of infected people; however, the article cited the cycling of infected people from facilities back into the hospital and again into nursing facilities.
- The most basic measures for hygiene play a significant role in preventing the spread of infection; nevertheless, in certain cases even the use of latex gloves, disposable gowns, masks, and hand sanitizer were forgone.
As a result of lapses in infection control measures, seriously ill patients—as well as their family, their friends, and the public at large—are at greater risk for contracting infections that are all but impossible to cure.
Ensure Your Loved One’s Facility Meets Staffing and Training Standards
When seeking a Pennsylvania, Philadelphia, or New Jersey nursing home, it’s important to be sure the facility is well staffed and properly trained in matters of contagious infections. If you are seeking an elder care facility for a loved one and need advice on how best to choose a Pennsylvania, Philadelphia, or New Jersey nursing home, or if you suspect staffing issues or poor care has led to an instance of neglect or abuse at a Philadelphia/PA or NJ facility where your loved one lives, please contact nursing home abuse attorney Brian P. Murphy to discover your legal rights and options.